Pancreatitis is a serious condition that results in inflammation of the pancreas. There are two types – acute and chronic. Acute pancreatitis comes on without warning. Chronic pancreatitis occurs over a long period of time.
What are the symptoms of acute pancreatitis?
It causes severe pain in the upper abdomen and back. There is often associated vomiting. The pain can be so severe that it makes people believe they are having a heart attack. Almost all patients with pancreatitis will present to a hospital. Often the pain can be made better by leaning forward.
Chronic Pancreatitis presents as episodes of abdominal pain that come and go. This pain may occur every day. There may be diarrhea and diabetes.
What causes pancreatitis?
The most common causes of pancreatitis in Australia are gallstones or alcohol. There are many rarer causes such as surgical procedures, high cholesterol, medications, viruses, inherited abnormalities and tumours.
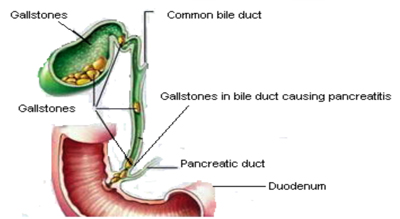
Gallstones are thought to cause pancreatitis by escaping from the gallbladder and passing through the common bile duct. They then block the pancreatic duct and set-off inflammation in the pancreas. Approximately 70-80% of these gallstones will then pass on into the bowel. Unfortunately the damage to the pancreas carries on.
Alcohol causes its damage via a direct toxic effect on the pancreas. Alcoholic pancreatitis is much more likely to leak to chronic pancreatitis especially if the patient continues to drink.
How is pancreatitis diagnosed?
Pancreatitis is diagnosed with a blood test called Lipase. If this is markedly elevated it is likely you have pancreatitis. The doctor will then look for the cause. Alcohol can obviously be ruled in or out by asking you about your alcohol intake. All patients with a first attack of pancreatitis must have an ultrasound looking for gallstones.
Is there any treatment for pancreatitis?
Unfortunately, we have not discovered a way to turn off the inflammation that occurs in pancreatitis. The only treatment available is to support the patient through an attack with oxygen, intravenous fluid and pain relief. The cause of the pancreatitis should be removed as soon as practical after the attack. These treatment decisions can be very complicated.
What tests can I expect to have?
You may initially have blood tests and some simple x-rays in the emergency department. You can also expect to have an ultrasound to look for gallstones. A CT scan in usually performed a few days into the attack when the kidneys are functioning better, to look for the complications of pancreatitis.
How long will it take to get better with pancreatitis?
When the pancreas becomes inflamed, alkaline juices pour out and begin to digest the pancreas and surrounding fatty tissue. This in turn produces toxins in the blood that have wide-ranging effects on the entire body. Pancreatitis affects the lungs, kidneys, liver and heart. There are various ways for doctors to figure out how severe an attack of pancreatitis is. In other words, the way a patient behaves in their first 24 hours of admission can predict how bad it will all be and what complications may ensue. Mild pancreatitis is likely to occur only once (if the cause is fixed) and you can expect to recover in 1-2 weeks. Moderate or severe pancreatitis can keep you in hospital for many weeks or even months and can be a life changing event for you and your family. I will discuss the treatment of mild and severe pancreatitis separately.
Treatment of mild pancreatitis
The aims of treatment are to support your vital functions. You will be given fluid via a drip in your hand, oxygen and appropriate pain relief. Pancreatitis is usually very painful and often requires narcotic pain-relief. You will only be able to drink small amounts of fluid, because resting the bowel is thought to aid in recovery. Patients with pancreatitis will not usually feel like eating. A diet will be introduced as you feel better and the nausea settles. It is normal for your bowels to not work for a week or more with pancreatitis. Your blood sugars will be monitored. It is common to get temporary diabetes. There is a procedure called ERCP (endoscopic retrograde pancreatography) that is occasionally recommended for patients with pancreatitis. A telescope (endoscope) is inserted via the mouth and into the stomach. Gallstones are then extracted from the common bile duct internally. The decision to do this test is a complex one and will be discussed with you if it is felt necessary. If your pancreatitis has been caused by gallstones, as soon as you start to improve, surgery to remove your gallbladder will be scheduled. This is usually done via keyhole surgery, but may require an open operation. If your pancreatitis is due to alcohol, you should not drink alcohol again for ANY REASON – not Christmas, not birthdays, not anything. If you do, you are likely to get ongoing attacks of this excruciating pain and eventually completely burn out your pancreas. Even if your pancreatitis is due to gallstones, drinking alcohol is not a good idea.
Surviving severe pancreatitis
For the family
It is very important that the family of the patient with pancreatitis reads this section. The patient will be too sick to understand anything and for many families, severe pancreatitis changes the course of their loved one’s life for many months. To many of you, the rapid onset of this disease will be astonishing. You go from well one day to a life-threatening illness the next. It will be a long and rocky road for you and I will attempt to keep you as informed as possible. This is a very complicated condition to understand, with many delicately timed decisions to be made. Severe pancreatitis affects all the organ systems in the body. It can be so serious that it can kill within 24 hours. Its treatment can require several weeks and even months in the hospital, multiple scans, procedures and operations. This can be followed by months in rehabilitation.
The management of pancreatitis is all about timing. The difficulty for the family – is that everything moves very slowly. Modern treatment of pancreatitis involves supporting the body while it fixes itself. We have learned by hard experience that intervening too early can be to the patient’s detriment. The most common question I am asked on the first day is – “why can’t you just remove the pancreas.” The answer is – because you can’t. Once the biochemical process of tissue destruction has begun, it cannot be reversed. The pancreas liquefies and develops gangrene very rapidly. Operating at this time would result in bleeding and death. It is possible to live without the pancreas, but it is a difficult life.
Let me start at the beginning and try and walk you through what you may expect in a course of severe pancreatitis. On admission, your loved one may be so sick that they require immediate admission to Intensive Care. They may already have breathing difficulties and require support on a ventilator machine that will breathe for them. For many, this lung failure comes further down the track. The kidneys may not be working very well, but usually intravenous fluids will help with this. Occasionally dialysis is needed (the blood is removed from the body and “washed” by a machine to remove toxins.) If the patient is awake, they may have a lot of pain. This will be managed with narcotic pain killers like Morphine. The patient may have a high fever and be jaundiced. If they are jaundiced they may have an ERCP (endoscopic retrograde cholangiopancreatography) on admission to take the gallstones out of the bile duct and relieve the pressure in the system. There will be a CT done when the patient is stable. Patient develop severe pancreatitis because the pancreas loses its blood supply and dies. The CT scan will give me an idea of how much of the pancreas is affected.
Nutrition is very important in the management of severe pancreatitis. The bowels stop working for a period of time. This makes feeding by mouth impossible. As soon as practical a special IV line will be inserted in the arm and feeding via the intravenous route will begin. Even with this type of feeding – patients can expect to lose 10-30 kg in weight with severe pancreatitis. From here it is a watch and wait situation. As soon as the patient is well, we schedule surgery to remove the gallbladder. Patients often take a backward step after this for a short time, because the toxins in the dead pancreatic tissue are stirred up. After that, we provide continued support. Removing the gallbladder does not put a stop to the pancreatitis. Many more complications can occur.
Your loved one may require surgery for a buildup of fluid behind the stomach called a pseudocyst. This surgery commonly occurs many months after an attack. Many weeks after a severe attack – several life threatening complications can occur. There may be a sudden rupture of the artery supplying the spleen. This will cause massive bleeding and shock. The patient will need emergency surgery to remove the spleen or intervention in the x-ray department. The second problem occurs when the gangrene in the pancreas develops a massive bacterial infection. This often requires multiple surgeries to remove all the infected tissue. During this time, the patient’s abdomen may remain open.
All of this is very difficult for families to understand. I will keep you informed about what is going on. Time off work – the patient with severe pancreatitis will require several months off work. I am happy to fill out any income protection paperwork you need.
Activity
You can expect your nurse and physiotherapist to help you get out of bed every day. You will be helped to walk short distances even with all of the tubes and intravenous lines. This is extremely important to prevent pneumonia, clots in the legs and loss of general condition. You can expect to have to wear stockings on your legs whilst in hospital to prevent clots and have an injection of heparin twice a day under the skin for the same reason. Clots to the lungs are a life threatening problem in pancreatitis.
Other Important Information
You can expect to see your surgeon every day. On weekends or in times when your surgeon is operating elsewhere, you will see one of the practice partners. All are very experienced in the treatment of pancreatitis. We will make every effort to keep you informed of your progress. We are always honest and open with you and your family. Feel free to ask questions.
Length of Stay in Hospital
As discussed, this is very variable. Mild pancreatitis may get better within a day or two. With severe pancreatitis – it is not uncommon to be in the hospital and then rehabilitation for 3 months even up to a year. It will have a life changing effect on the patient and the family.
What are the possible complications associated with pancreatitis?
While the majority of cases of pancreatitis get better completely with no ongoing problems, a small number develop serious complications as discussed previously. This is a list of the potential problems that can be encountered. These complications are not predictable and do not occur in everybody. Discussion with your surgeon is the best way to understand these problems. I only include this list to prompt discussion and not to frighten.
- Jaundice and bile duct infections: caused by gallstones in the bile duct.
- Diabetes: if it is going to occur, it happens early in the attack. In most patients with mild pancreatitis this resolves. Patients with severe pancreatitis, tend to end up with permanent diabetes as part of the pancreas dies.
- Diarrhoea: the pancreas produces juice to help the body absorb fat. After severe pancreatitis the pancreas no longer produces this juice. This results in fat in the bowel motion, that in turn causes diarrhea. This can be easily be rectified with pancreatic enzyme tablets.
- Pancreatic pseudocyst: when the pancreas is inflamed – like any raw surface, it weeps a clear fluid. In the belly, this fluid gets trapped in the space behind the stomach. This is called a pseudocyst. There can be one fluid collection, or there may be many. They often go away with no treatment. If they are large, they tend to need drainage. Pseudocysts cause problems by placing pressure on the organs next to them. The most common problem is pressure on the stomach – stopping the patient from eating and even leading to vomiting. The timing of draining these cysts is a complex decision. They may be drained at an operation, via a telescope passed through the mouth (endoscopy) or in X-ray with a needle through the skin.
- Bleeding: this bleeding can be gradual or may be sudden and life threatening. Gradual bleeding occurs as the inflamed pancreas causes the blood vessels around the pancreas to become leaky. It is common in severe pancreatitis to need “top-ups” with blood. A feared complication of severe pancreatitis is rupture of the artery that supplies the spleen. This happens with no warning and occurs several weeks after the initial attack. It only occurs in severe pancreatitis and usually the patient is still in the hospital where medical help is at hand.
- Infection of the pancreas. Like anything dead, infection with bacteria is a significant risk. Antibiotics do not prevent this. If infection of the dead pancreas occurs – surgery is often required.
- Surgery for severe pancreatitis often has to be repeated many times until all the dead pancreas is removed. This may result in the patient’s abdomen being left open. When things are inflamed, the tissues get very swollen. This makes it impossible to close the belly. In the end – this causes a large hernia that needs to be fixed many months later. Another consequence of an open belly is that holes may develop in the bowel and cause bowel fluid to leak out of the belly. This is a difficult problem, but can eventually fixed over time.
- Clots in the legs and lungs: measures are taken to prevent this but it still occurs and can be fatal.
- Complications related to IV lines and feeding tubes: patients with severe pancreatitis require many IV lines to support their recovery. These lines are placed in large veins and cause infections, clots and punctured lungs.
- Depression: like all severe illness – pancreatitis has a huge impact on the mental state of the patient and their family.
- Death from any cause: up to 30% of patients with severe pancreatitis will sadly die of the disease.
Weight loss:
it is common to lose up to 20% of starting body weight after severe pancreatitis. (approx. 10-20kg)
What does the pancreas do?
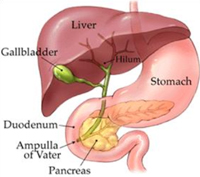
The pancreas is in the upper abdomen and is draped over the backbone. Pain related to the pancreas often presents in the back. The pancreas has two functions.
- It produces insulin and other hormones to prevent you getting diabetes.
- It produces digestive juices to help your body breakdown your food. These juices drain into the duodenum (bowel). They do not become “activated:” until they enter the bowel.
