Common reasons to have this operation are cancer of the head of the pancreas, bile duct, duodenum or ampulla. For these cancers, Whipple’s operation offers the only chance of cure.
There are also many non-cancerous conditions that are treated with this procedure: eg. cysts of the head of the pancreas and bile duct, pancreatitis, pre-cancerous tumours, trauma and rarely even for gallstones lodged in the head of the pancreas.
It should be noted, that it is sometimes difficult to obtain an absolute diagnosis of cancer either before or even during the surgery. The pancreas tends to develop a great deal of scarring or reaction that interferes with interpreting a pre-operative needle biopsy. It is common to biopsy a cancer in this region and obtain a benign result. Thus, it is up to the surgeon’s judgment whether or not there is cancer present and if a Whipple’s Procedure would be of benefit.
The presence of cancer in the piece of tissue removed is determined by the pathologist when they look under the microscope. A result from the pathologist can take anywhere from 2 – 7 days.
The decision to proceed to this type of surgery is very complicated. This is the reason that it is important to be operated on by a surgeon with a great deal of experience in surgery for cancer of the pancreas and bile duct. His/her judgment will be valuable in determining whether or not a tumour is present and if it is removable.
Sadly, sometimes during surgery the surgeon will determine that the cancer is not removable. This is often due to the finding of secondary cancer in the liver. Another reason may be the cancer’s relationship to important blood vessels supplying blood to the liver and bowel. These blood vessels cannot be removed without threat to the patient’s life. If the cancer is not removable, the surgeon may elect to perform a biliary bypass procedure to permanently drain away the jaundice. This will be discussed fully with you and your family after the surgery.
The operation
The Whipple’s procedure is performed in two stages:
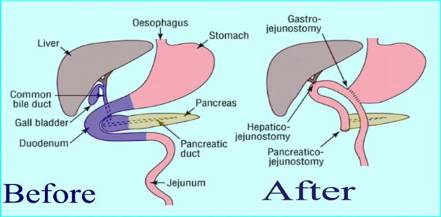
- Removal stage: The gall bladder (cholecystectomy), the common bile duct (choledochectomy), the head of the pancreas, duodenum, part of the stomach, part of the small bowel and the lymph glands in the area are remove.
- Reconstruction stage: The pancreas is attatched to small bowel, the bile duct joined to the bowel and finally the stomach is attatched to the bowel to allow food to pass through.
What to expect immediately after surgery
Pain Relief
In the first few days after surgery there may be a moderate amount of discomfort.
You will have some form of pain relief. There will be a choice of:
- epidural (if medically suitable)
- Patient controlled analgesia (PCA) and painbuster – a button to press that delivers strong pain killers into your IV combined with a tiny catheter in the wound providing local anaesthetic.
Your anaesthetist will discuss the pros and cons of each with you prior to surgery and it is your choice in conjunction with your anaesthatist. Either option may not be suitable for every person.
Every effort will be made to minimize the discomfort and make it bearable. Your treating team will be monitoring your level of pain frequently.
When you are back on a normal diet, you will be converted to oral pain relief.
Drain tubes
You will have a number of plastic tubes in your body following surgery. They will vary a little depending on your particular medical need. They will be removed at variable times following your surgery under the direction of the surgeon. All tubes except for an IV in your hand will be placed under anaesthesia.
- IV line: Central venous line placed in your neck (done under anaesthesia) to give you fluids and pain relief after surgery.
- Urinary catheter: tube placed in your bladder so you don’t have to get up to pass urine.
- Abdominal drain tubes: two or three soft plastic drains coming out of your abdomen that are placed around the pancreas to drain any fluid, bile or pancreatic juice, so it does not collect in your abdomen.
- Stomach/small bowel feeding tube: a double barrelled tube that sits in your small bowel and stomach and emerges through the skin. It has the dual function of draining fluid from your stomach whilst feeding your small bowel with high energy food. This tube is not used in all cases.
- Nasogastric tube: some patients require a tube that goes from their nose into their stomach. This tube is not used in all cases.
Eating
You will not have anything to eat or drink for several days after surgery. An intravenous infusion will provide you with the necessary fluids. In some cases you will have a nasogastric tube (NG) in your nose that will remove the stomach contents until your stomach and intestines recover. A feeding tube called a jejunostomy tube may be inserted to help with feeding after the surgery. Your surgeon will let you know when you will be able to eat.
Urinating/Bowel Movements
In the first few days after the surgery, a tube placed in your bladder will drain your urine. You will probably not have a bowel movement until several days after the surgery.
Intensive Care
It is likely you will be looked after in intesive care for at least the first day after your surgery. Your continued stay here will depend on your condition.
Activity
You can expect your nurse and physiotherapist to help you get out of bed on the first day after surgery. You will be able to walk short distances even with all of the tubes and intravenous lines. As each day passes your tolerance for walking and sitting in a chair will increase. This is extremely important to prevent pneumonia, clots in the legs and loss of general condition. You can expect to have to wear stockings on your legs whilst in hospital to prevent clots and have an injection of heparin twice a day under the skin for the same reason.
Your Incision
You can expect to have a waterproof bandage over your incision for the first several days. Your surgeon will remove the dressing at the appropriate time. You will be able to shower with the waterproof dressing on. It is quite common to have a small amount of leakage from the wound.
Most commonly, you will not have any stitches to remove, they will be of the dissolving type.
Other Important Information
You can expect to see your surgeon every day. On weekends or in times when your surgeon is operating elsewhere, you will see one of the practice partners. All are very experienced in this type of surgery and commonly assist each other in the operating theatre.
We will make every effort to keep you informed of your progress. We are always honest and open with you and your family. Feel free to ask questions.
Length of Stay in Hospital
On average most patients will expect a 2-3 week hospital stay. This time however differs greatly for individual patients. Some stay shorter, some stay much, much longer. You will not be discharged before you can walk unaided and care for yourself.
What are the complications that may happen immediately after surgery for Whipple's procedure?
The Whipple’s operation is a complex surgery with many potential complications. In the hands of surgeons who are experienced, the complication rate is usually very low.
The most serious and specific complications that may be seen after this operation include:
Pancreatic Fistula
After the tumor is removed from the pancreas, the cut end of the pancreas is stitched onto the bowel so that pancreatic juices can mix with food to allow absorption. The pancreas is a very soft and sometimes fatty organ. In some patients, this stitching may not heal very well. If this happens, then a leakage of pancreatic juice into the abdomen occurs. A significant pancreatic leak occurs in 10-20% of patients.
Often, this leak is controlled by the soft plastic drain that the surgeon leaves at the time of the surgery, without any ill effect to the patient. In most patients who develop a leak of pancreas juice, the leak heals on its own.
Occasionally the drain doesn’t cope with all the drainage and the patient will need to be re-operated on to drain the pancreatic juice. This re-operation occurs in 1-4% of patients undergoing Whipple’s procedure.
Gastroparesis – paralysis of the stomach
It is quite common (about 25% of patients) for the stomach to remain paralyzed for a variable time after a Whipple’s operation. The small bowel however begins to function in the first one to two days after surgery.
It may take up to 4-6 weeks for the stomach to adapt to the changes after the surgery. This may mean that you cannot take anything by mouth during this time and you will have to remain in the hospital. It also may mean that you may require continuous drainage of your stomach to prevent vomiting. (Done with a tube in the nose, or a tube through the skin of your abdomen into your stomach)
If you experience a prolonged period of time where your stomach does not work, it can be emotionally very difficult time for you and your family. It is easy to loose spirit and feel quite “down”. Rest assured, the stomach will start working again in its own time and when this occurs it usually does so rapidly.
Other immediate complications and implications of this surgery
Like all major surgery there are a number of serious complications that may occur. These must be dealt with on a case by case basis. Some of these complications are:
- Death from any cause: approx. 1% of all patients having this type of operation.
- Bleeding: either in the first 2-3 days requiring return to surgery or delayed bleeding from a ruptured artery some weeks after surgery. You may require a blood transfusion.
- Other blood vessel problems: heart attack or stroke.
- Development of diabetes requiring insulin injections.
- Infections: Wound, pneumonia, urine, bile duct, intra-abdominal, epidural related, IV line related, related to the gastrostomy tube.
- Punctured lung secondary to the IV line in your neck.
- Clots in the legs that may travel to the lungs.
- Stomach ulcer that may or may not bleed. This may resent as a vomit of blood or black bowel motions.
- Urinary catheter complications: unable to pass urine after catheter removed especially in men
- Weight loss: it is common to loose about 10% of starting body weight after this surgery. (approx. 5-10kg)
- Wound pain and prolonged numbness under the wound.
- Hernia of the wound.
- You may require a blood transfusion (approx. 20% of patients having this surgery).
After discharge
What are the long-term complications of the Whipple operation?
Some of the long-term consequences of Whipple operation include the following:
Malabsorption
The pancreas produces a substance (enzyme) that digests food. In some patients, removal of part of the pancreas during the Whipple’s operation can lead to a decreased production of this enzyme. Patients complain of diarrhea that is very oily. Treatment consists of taking oral pancreatic enzyme pills and usually provides excellent relief from this problem. About 20% of all Whipple’s patients may require these supplements.
Diabetes
Another role of the pancreas is to produce insulin that controls blood sugar levels. During Whipple’s operation the head of the pancreas is removed. Therefore there is a risk of developing diabetes.
In general, patients who are diabetic before surgery or who have an abnormal blood sugar level controlled on a diet prior to surgery, have a high chance of their diabetes becoming worse. On the other hand, patients who have completely normal blood sugar prior to surgery with no history of diabetes and do not have chronic pancreatitis or morbid obesity, have a low probability of developing diabetes after the Whipple’s operation.
Alteration in diet
After a Whipple’s operation, we generally recommend that the patients eat smaller meals and snack between meals to allow better absorption of the food and to minimize symptoms of bloating or fullness.
Loss of weight
It is common for patients to lose up to 5 to 10% of their body weight after this surgery. The weight loss usually stabilizes very rapidly and many patients will regain this weight in the six months after surgery.
Passing drain tubes in bowel motion
During surgery, your surgeon may place several soft pieces of plastic tubing to hold open your bile duct and pancreatic duct. These may pass with your bowel motion at any time after your surgery. It is common not to notice them. If you do see them in the toilet, it is completely normal. DO NOT retrieve them from the toilet bowl.
How you may feel
You may feel weak or “washed out” when you go home. You might want to nap often. Even simple tasks may exhaust you. You may loose your taste for food.
You might have trouble concentrating or difficulty sleeping. You might feel depressed. These feelings are usually transient and can be expected to resolve in 2-4 weeks.
Your medications
Your surgeon will discuss with you which medications you should take at home. If needed, you will go home with a prescription for pain medicine to take by mouth.
Your incision
Your dressing will be removed before you leave the hospital and if it is not leaking it will be left open to the air. You may wear clothes over the top of it.
Your incision may be slightly red along the cut. This is normal. You may gently wash dried material around your incision and let water run over it. Pat the wound dry with a towel. Do not rub soap or moisturizer into your incision for at least 4 weeks or until it is fully healed. After this you may rub vitamin E cream along the wound.
It is normal to feel a ridge along the incision. This will go away. It is normal to have a patch of numbness under the wound.
You may see a small amount of clear or light red fluid staining your dressing or clothes. If it is minor cover that part of the incision with a pad. If leakage is severe, you should contact your surgeon.
Over the next few months your incision will fade and become less prominent.
Activity
Listen to your body, if it is hurting, don’t continue with the activity.
Do not drive until you have stopped taking narcotic pain medication and feel you could respond in an emergency.
You may climb stairs.
You may go outside, but avoid traveling long distances until you see your surgeon at your next visit.
Don’t lift more that 10 kg for 6 weeks. (This is about the weight of a briefcase or a bag of groceries) This applies to lifting children, but they may sit on your lap.
You may start some light exercise when you feel comfortable.
You may swim after 4 weeks
Heavy exercise may be started after 6 weeks – but use common sense and go slowly at first.
You may resume sexual activity when you feel ready unless your doctor has told you otherwise.
Costs to be incurred from this surgery
The surgeons in this practice do not charge any out of pocket expenses for your surgery. We will bill your health fund directly.
This may not apply to your anaesthetist. Ask your surgeon ahead of time who your anaesthetist will be.
We use a drug after your surgery called Octreotide to slow down the juices made by the pancreas. It incurs and out of pocket expense of $300-400. We feel that this decreases the risk of pancreatic leak. Please let us know if you do not wish for us to use this drug.
What does the pancreas do?
- It produces insulin to prevent you getting diabetes
- It produces digestive juices to help your body breakdown your food.
